WEHI receives WHO designation
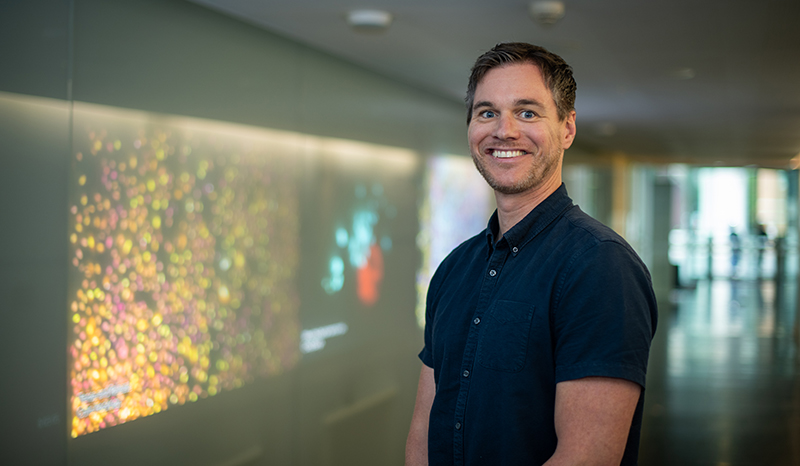
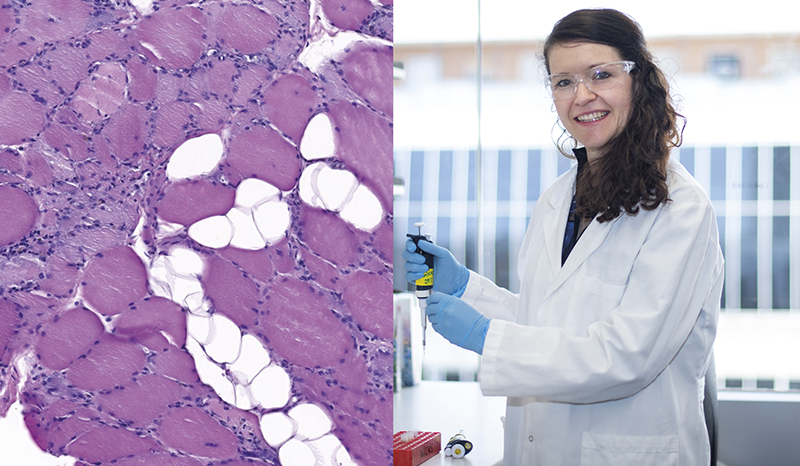
The designation enlists WEHI researchers, led by Associate Professor Sant-Rayn Pasricha, to support WHO to determine the best approaches and policies to diagnose and treat anaemia and recognises the expertise of WEHI researchers in combatting anaemia.
Associate Professor Pasricha said the WHO Collaborating Centre designation would enable researchers from WEHI to support the activities of the WHO and generate the knowledge needed to form guidelines and advice to countries throughout the world.