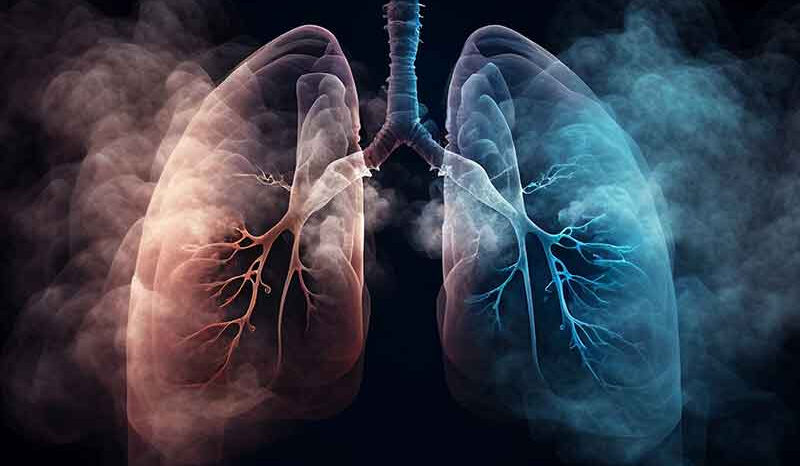
Lung cancer is the abnormal, uncontrolled growth of lung cells. This is caused by changes to their genetic material. Different types of lung cancers arise from different cell types within the lung. The process by which this occurs is poorly understood.
Most lung cancer types are classified by their microscopic appearance. These include:
- Small cell lung cancer
- Non-small cell lung cancer: squamous cell carcinoma, adenocarcinoma and large cell carcinoma.
Other types of cancer can also occur in the lung. Some of these are rare types of cancer that arise from lung tissue.
Of lung cancers in Australia:
- 10% are small cell lung cancers.
- 60% are non-small cell lung cancer.
- 30% are rare types of lung cancer or cannot be definitively classified.
Cancer cells from other organs can also spread (metastasise) to the lung.
Mesothelioma is a type of cancer that starts in the lining of the chest and spreads into the lungs. Exposure to asbestos is strongly linked to mesothelioma. For more information about mesothelioma, please visit Cancer Council Victoria.
The treatment and outlook for lung cancer depends on the type of cancer, and how far the cancer cells have spread. Lung cancers may be:
- Contained within one part of a lung.
- Spread to several sites across the lungs.
- Spread (metastasised) to other parts of the body.
Most cases of lung cancer in Australia are detected at later, harder-to-treat stages.