Lymphoma is a cancer that develops from white blood cells called lymphocytes. It occurs when a lymphocyte undergoes changes that allow it to divide uncontrollably and become long-lived.
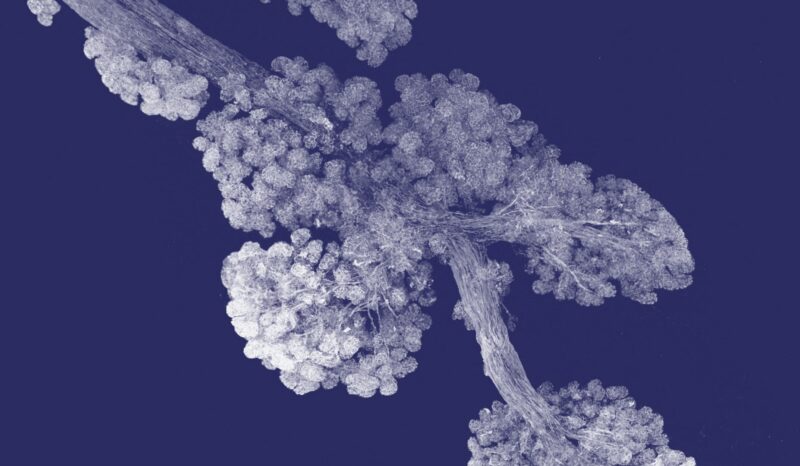
Lymphoma develops within the lymph nodes, spleen, or bone marrow, collectively called lymphoid organs. The lymphoma cells initially grow within a single lump. Over time they may spread to other parts of the body.
Lymphoma shares many similarities with some types of leukaemia.
There are many types of lymphoma. These differ in:
- The features of the lymphoma cells, such the proteins found on the outside of the cells.
- The location of the lymphoma within the body.
- How rapidly the disease advances.
- The best treatment for the particular lymphoma.
- The characteristics, such as age, of the people who are most often affected.
Research is revealing how different types of lymphoma develop. Many occur because of changes in the genetic material of certain types of lymphocytes. For example, follicular lymphoma cells contain a genetic rearrangement that increases the amount of the cell survival protein Bcl-2 in cells.
Some lymphomas are triggered by a viral infection. Some types of lymphoma are associated with Epstein-Barr virus (EBV), although most people who develop this common infection never get lymphoma. The virus introduces its own genetic material into lymphocytes. This may trigger the lymphocyte to divide uncontrollably or become long-lived.
Lymphoma Australia and the Leukaemia Foundation provide information about specific types of lymphoma.