The immune system’s role is to attack anything that poses a threat to health, such as bacteria and viruses. During development, the immune system usually learns to ignore things that are harmless, such as food and pollen.
Some people, however, respond to harmless substances as if they were a threat, leading to a damaging immune response called an allergy. The substance that triggers the immune response is known as an allergen. People with a family history of allergy and asthma are at greater risk of developing allergies.
Common allergens include:
- Foods, for example peanuts, cow’s milk, eggs, shellfish
- Medicines, for example antibiotics
- Dust mites
- Pet urine, saliva or dead skin cells
- Pollen
- Insects
- Ticks
- Moulds
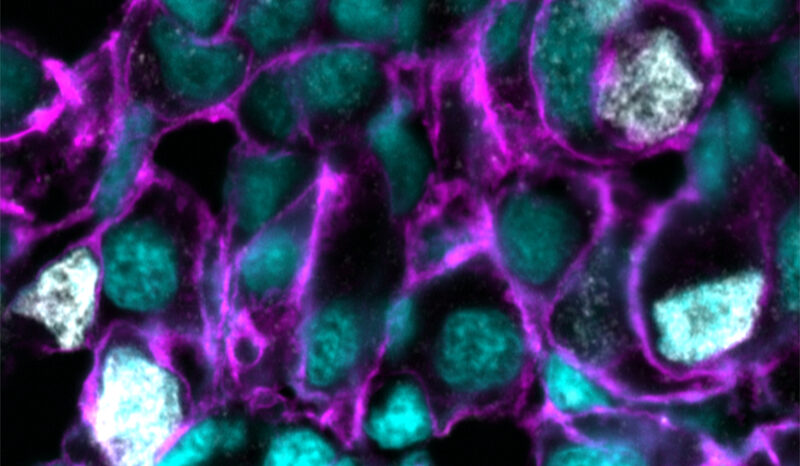
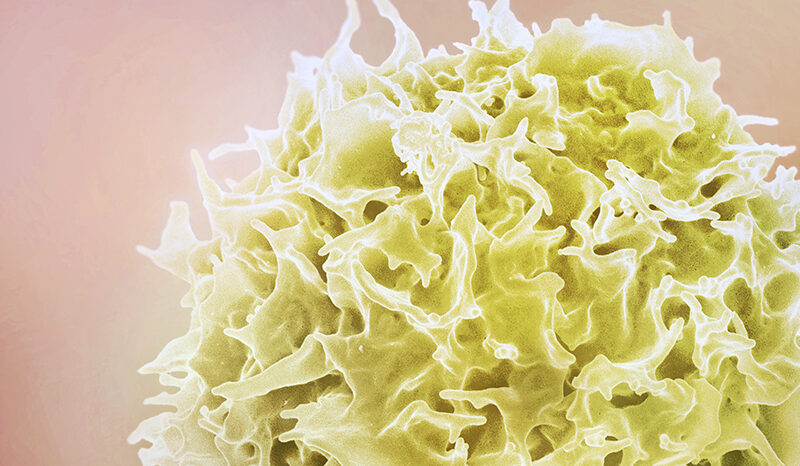
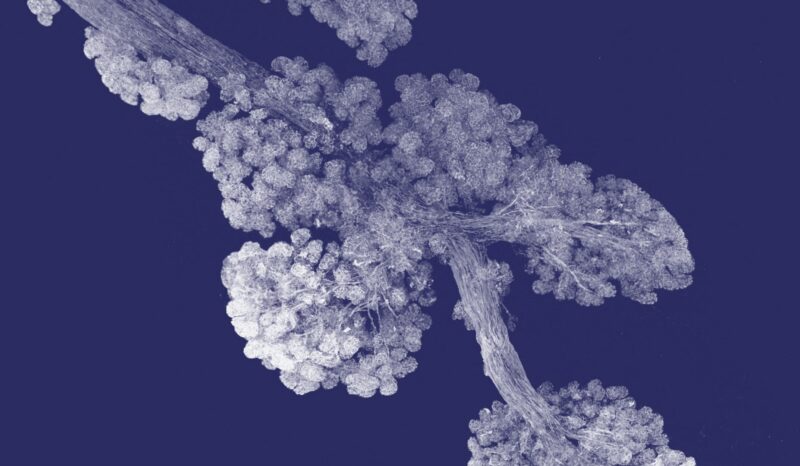
During an allergic response, the immune system produces a protein called immunoglobulin E (IgE). The IgE binds to specialised immune cells called mast cells, triggering the release of chemicals such as histamine that cause allergy signs and symptoms.
Coeliac disease is sometimes referred to as a gluten or wheat allergy, but it is not IgE-mediated and instead involves different parts of the immune system.