Asthma is a common inflammatory disease of the airways.
Normally the airways are open and relaxed, allowing air to easily move in and out. People with asthma have sensitive airways that are primed to react to triggers in the environment, leading to an asthma attack.
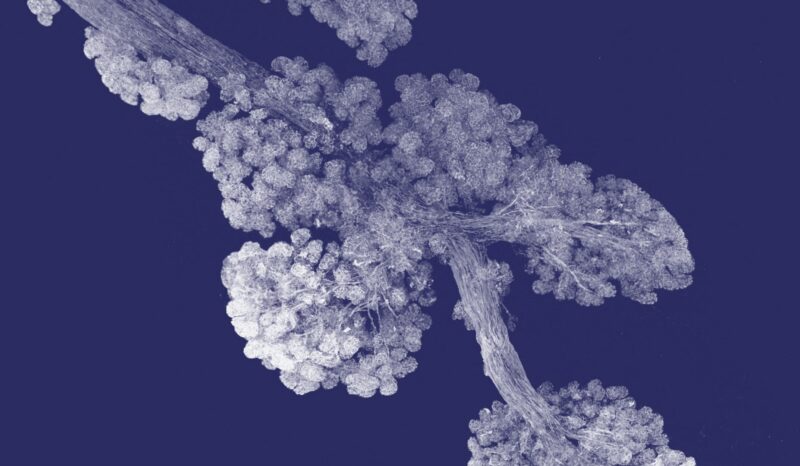
The triggers that bring on an asthma attack vary between different people. Asthma is often triggered by the immune system responding to inhaled substances such as pollen, house dust mites and mould spores. Asthma attacks can also be triggered by the common cold, exercising, or by environmental irritants like cigarette smoke and pollution.
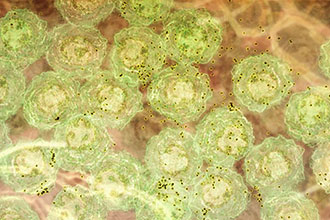
During an asthma attack, the airway lining becomes swollen, inflamed and thick with mucous. The muscles in the airways tighten, narrowing the airways. These changes restrict airflow, making it difficult to breathe.
Asthma attacks can come on gradually or quickly. When asthma occurs as an acute attack, the airflow restriction can be life threatening. Each year approximately 400 people in Australia die from asthma.