Almost all people with type 1 diabetes rely on insulin injections for their entire lives. They must closely monitor their blood glucose levels. When blood glucose rises, such as after a meal, an appropriate insulin dose is calculated and injected. Insulin is available in ‘slow acting’ and ‘fast acting’ forms. These can aid the smoother control of blood glucose levels.
There is no orally available (tablet) form of insulin. Insulin can only be given by injection, such as with a syringe. Recently, small, attachable insulin pumps have been introduced instead of multiple daily injections. Insulin pumps may control blood glucose better by providing a more steady release of insulin into the body.
The only cure for type 1 diabetes is transplantation or regeneration of insulin-producing cells.
Transplantation of the whole pancreas or the parts of the pancreas containing insulin-secreting beta cells can be performed. It is limited by a shortage of organ donors, and the need for life-long immune suppression to prevent transplant rejection. Thus, transplantation is restricted to people with poorly controlled diabetes and serious complications.
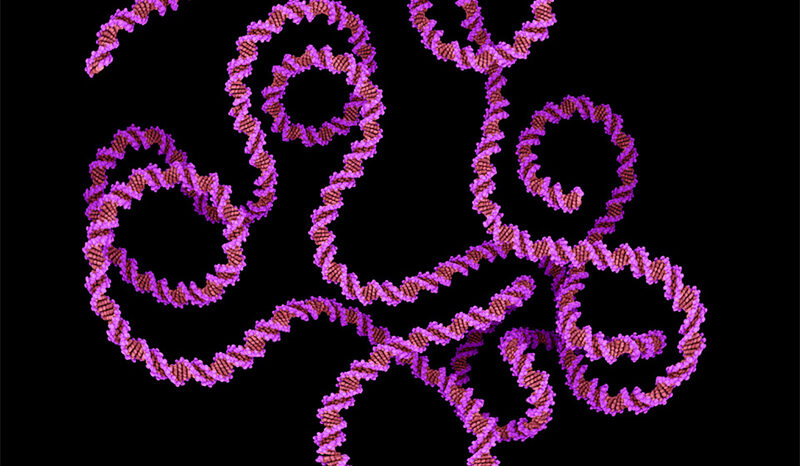
Our researchers have shown that the pancreas contains stem cells that can be transformed into beta cells. Their hope is that it may one day be possible to cure type 1 diabetes by stimulating the regrowth of beta cells. This would depend on stifling the immune cells that originally destroyed the beta cells.
Diabetes Australia has more detailed information about diabetes treatment.